The New Zealand abortion law changed significantly in 2020 with the passage of the Abortion Legislation Act 2020.
This law allows abortion on demand up to and including 20 weeks of pregnancy. After 20 weeks a woman may obtain an abortion if her doctor or other qualified clinician (midwife, nurse practitioner, registered nurse) believes the abortion is ‘clinically appropriate’, and that continuing the pregnancy would endanger her 'wellbeing’. The clinician has to consult with another doctor / appropriate health professional. Both terms, 'clinically appropriate’ and 'well-being’, are not objectively defined. Therefore, abortion is in effect available on demand up to birth.
The previous law that was struck down in 2020 only allowed abortions after 20 weeks in order to save the life, or prevent serious permanent mental or physical harm of the mother. It also required an agreement and approval of two doctors.
This new law has widened the parameters for abortion significantly in New Zealand and is now one of the most liberal abortion laws in the world.
New Zealand Abortions Statistics
Weeks 0-20
Weeks 21-40
Unknown / Missing
Medical Abortions
Surgical Abortions
Other*
Unborn children aborted in NZ in 2020
Weeks 0-20
Weeks 21-40
Medical Abortion
Surgical Abortion
Other*
*(e.g. failed medical only followed by surgical)
What is the abortion law in New Zealand?
Understanding how this fails the woman and her child
Medically Failing Us
The dangers with abortion
The only measures for an abortion up to birth is a doctor’s decision that it is 'clinically appropriate’ or for the mothers 'well-being’. Our previous abortion law stipulated that a woman could receive an abortion up to 20 weeks gestation on the grounds of ‘mental health’ risks. We saw this previous law abused and many abortions were signed off under the ‘mental health’ banner. This too will happen with abortions after 20 weeks, as it will be just as easy for someone to claim that their pregnancy affects their ‘wellbeing’, which is even more subjective than ‘mental health’.
Many amendments and safeguards were rejected in the parliamentary process. Amongst the rejected safeguards are the following:
- No protection against gender-selective abortions. The amendment to make gender-selective abortions illegal was rejected.
- No protection against disability discriminatory abortions. The amendment to protect babies with a disability from discrimination was rejected.
- No medical assistance for a baby who survives a botched abortion attempt. An amendment to ensure that medical assistance should be provided to a baby born alive after a failed abortion was rejected, meaning that abortion survivors will be legally left to die. Under the NZ Bill of Rights, a survivor of abortion is legally entitled to care, this would be another breach of human rights.
- No protection against a mother being coerced into an abortion. An amendment to ensure that a mother will not be forced or pressured into an abortion by a partner or family member was rejected.
- No pain relief to be given to a baby in a post 20-week abortion. An amendment to see that babies in a post 20-week abortion would not suffer any pain, was rejected even though it is scientifically proven that babies can feel pain in late term abortions.
- No protection for healthcare professionals to have conscientious objection. An amendment to ensure that we kept the same conscientious objection standards the same was rejected.
- No protection for health professionals to keep their job if they conscientiously object. An amendment to ensure restricting employment discrimination on the grounds of conscientious objection was rejected.
A Doctor’s Dilemma
Why health professionals want nothing to do with this
Abortion is not a healthcare service. Abortion is an intentional act of killing another human being. It is not a solution that cares for both lives involved in the pregnancy. Pregnancy in itself is not a ‘danger’ to a mother, and abortion is not a way to ‘fix’ or ‘heal’ a pregnancy. This goes against a doctor’s role of healing, as an abortion is a deliberate act of killing a child.
Abortion can harm the woman seeking an abortion. There are medical issues that can arise as a direct result of an abortion as well as emotional and mental health issues post abortion.
We have been led to believe that sometimes abortion is necessary if the mother’s life is in danger. This is not true. The act of aborting a baby is actually never medically necessary. Doctors have stated that on the rare occasion of a mother’s life being at risk, an induced labour to cause the baby to be born prematurely to save the mother's life is an adequate procedure. The baby may not survive the birth and although still a tragedy, this is very different to intentionally killing a baby while it is inside its mother’s womb, through abortion.
The fact is that there are two lives that need to be considered. When someone chooses to have an abortion, one of those lives is intentionally killed.
Prenatal development
The week by week development of a little human
“The start of pregnancy is normally marked by the first day of the woman’s last menstrual period (LMP). This is called the gestational or menstrual age. It is about two weeks ahead of when conception actually occurs.”
“Fertilisation. This is when a sperm enters an egg. All going well, the result is a new human being, at this stage referred to as a zygote. The zygote now begins a journey along the fallopian tube towards the uterus.”
“Implantation. At this point, the developmental stage known as a blastocyst burrows into the uterine lining. ”
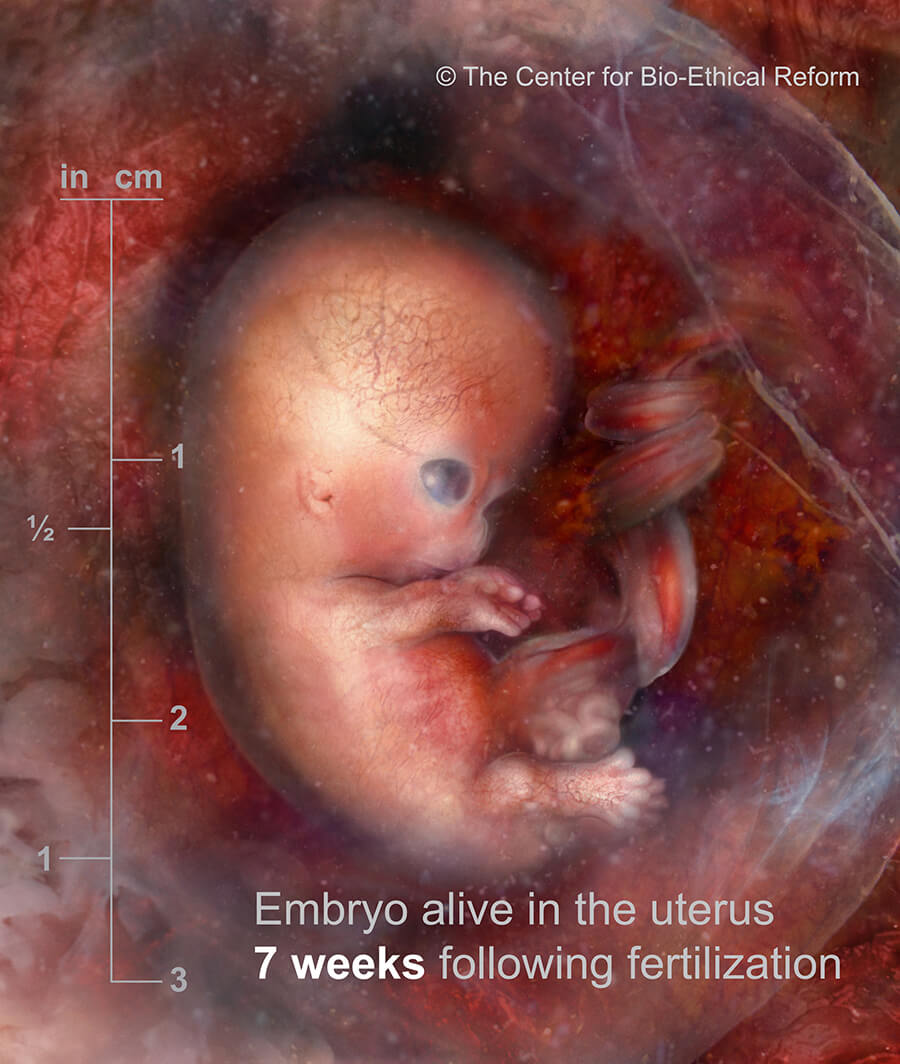
“ Embryo. At this stage a circulatory system is developing, as well as the foundations for the skin, bones, ligaments and kidneys.”
“The heart is beating. The neural tube from which the brain and spinal cord develop has now closed. Small buds have formed on the trunk; these will grow into the arms and legs.”
“Further development of the brain and face. The buds on the trunk are now resembling paddles.”
“The lower buds become more pronounced, developing into the feet. Little fingers are recognisable. Facial features such as nose, eyes, lips and ears are forming.”
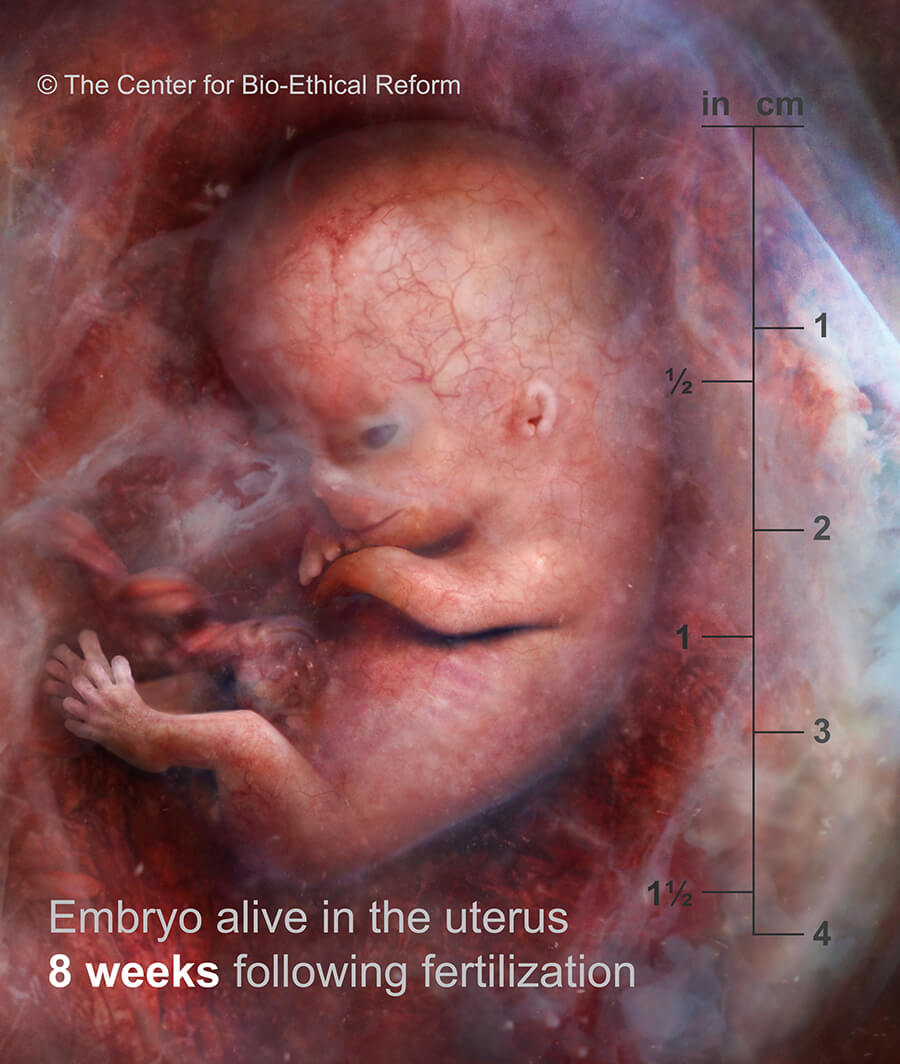
“Toes have formed. The head is much more pronounced. At this stage, the preborn child, known as a foetus, measures 16 – 18 mm.
9 weeks LMP”
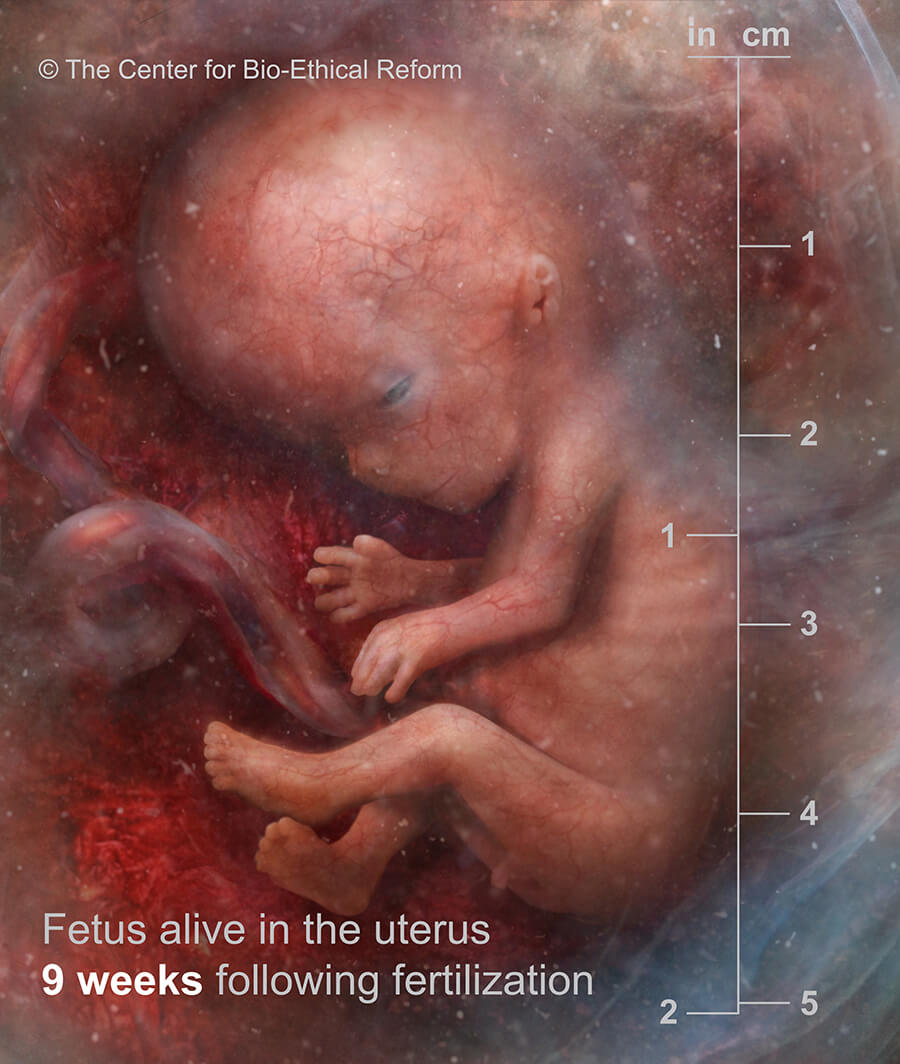
“The foetus can now bend their elbows and knees. The fingers and toes have lost their webbing.
10 weeks LMP”
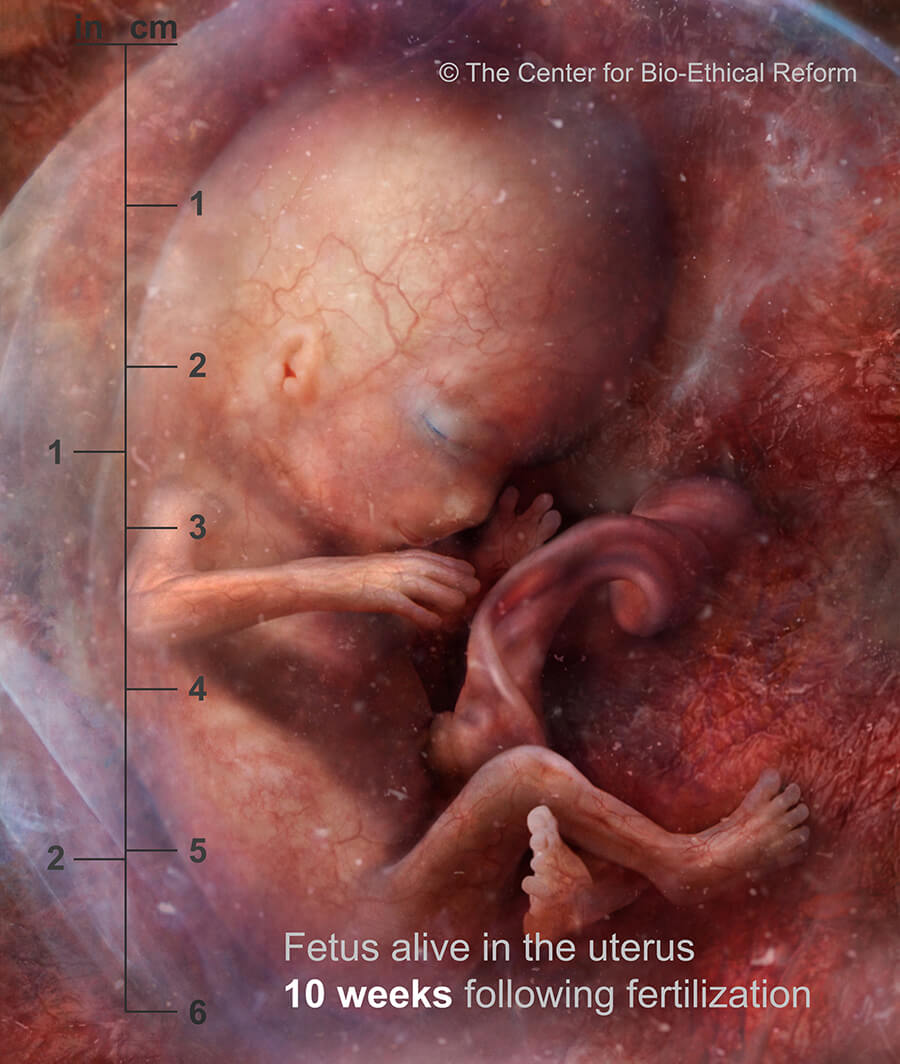
“External genitalia are developing. The liver is making blood cells. Tooth buds are emerging. The foetus is now practicing breathing motions.
11 weeks LMP”
“ The preborn child now has a very human looking facial profile and makes random movements. Fingernails are growing. The intestines have shifted into the abdominal cavity.
12 weeks LMP”
“All major organs are present, although not yet fully developed enough for survival outside the womb.”
“Toenails are developing.”
“Some women can feel their preborn child moving. At this point the average weight of a preborn child is 117gm, and their average length is 16cm. ”
“The lungs are developing quickly, although at this stage they are not yet filled with alveoli, the sacs in the lungs that allow gas exchange. ”
“Ears are now more pronounced and are folding out from the head. The preborn child begins to hear for the first time.”
“Facial features are now clearly recognisable.”
“There is now fine hair covering the body, known as lanugo. On average the preborn child is now 27cm long and weighs 400 gm. From this point, development is more about fine-tuning the organs and increasing in size and weight.”
“Rapid Eye Movement, an indication of dreaming, has been noticed at this stage. ”
“The preborn child is able to respond to sounds outside of their mother’s body. ”
“From this stage onwards, the preborn child is storing fat and further developing muscle tissue. ”
“The pregnancy is considered full term and the child will soon be born.”
Medical and Surgical Abortion
Understanding the different methods that are used
What happens in a medical abortion?
Understanding how a life is ended through this method
Medical abortion involves the woman taking the drug mifepristone known as Mifegyne® which blocks the pregnancy hormone progesterone. This causes the preborn child to be deprived of nutrients. Within the next 48 hours the woman takes another drug, misoprostol, known as Cytotec®, either orally or vaginally. This causes uterine contractions and the embryo and associated pregnancy tissues are expelled. This method is offered up to nine weeks LMP.
For late-term abortions in New Zealand, the abortionist usually initiates foeticide, which is killing the preborn child by injecting a drug into the heart to stop it. Labour is then induced and the woman goes through the delivery process.
What happens in a surgical abortion?
Understanding how a life is ended through this method
Surgical abortion in the first trimester is carried out using the dilatation and curettage (D&C) and vacuum aspiration method. It involves dilating the cervix and inserting into the uterus a small tube attached to a suction machine. Suction is activated and removes the preborn child and pregnancy tissue (the placenta and lining of the uterus).
After 14 weeks, due to the strength of the preborn child’s body, bones, and size in general, a procedure called dilation and extraction (D&E) is performed. This involves the use of suction as well as forceps to break the preborn child’s body and remove it in pieces.
What Abortion Looks Like
The Victims Speak
CAUTION: Viewer discretion and parental guidance advised. Contains graphic images of aborted children.
The Dangers in Abortion
Harms to the mother
Physical Harm
Abortion carries a risk of physical harm. The most common complication of abortion is infection. If untreated, it can pose a serious risk to fertility and even endanger the woman’s life. Surgical injury to the uterus or cervix is not uncommon, and can have a significant impact on the woman’s future health and fertility.
Conscious Sedation
Currently most abortions in New Zealand are done under conscious or twilight sedation, which means that the woman is sleepy but awake during the procedure. General anaesthesia, when the woman is unconscious throughout, can be provided in a hospital setting. General anaesthesia carries the usual risks of adverse cardiac or respiratory events, although these are quite uncommon.
Medical Risks
Risks from medical abortion include failure of the abortion drug to work, requiring a surgical abortion, and uncontrolled bleeding and infection. Allergic reaction is also possible.
Mental Health Risk
Because no one currently systematically tracks or checks in with women following an abortion, we can’t say for certain how many women are suffering after having an abortion. But a 2008 study out of the University of Otago’s Christchurch Health and Development Study suggests that women who have an abortion face about a 30% increase in the risk of developing mental health problems – such as depression, anxiety disorders, suicidal behavior, and drug and alcohol abuse – versus women who have never had an abortion, and that this increase is associated with having the abortion.
Long Term Effects
Anecdotal evidence from counsellors indicates that women can experience mental health problems as a result of their abortions anytime from immediately after the abortion to many years later.
Do You Need Help?
What you are going through matters to us
Be a Voice for the Voiceless
How to get involved